
Hospitals, healthcare, and wellness clinics are navigating a relentless balancing act: improving health outcomes, meeting ever-tightening regulatory demands, and cultivating lasting patient loyalty, all while staff bandwidth shrinks. Against that backdrop, patient feedback has emerged as one of the few forces capable of bridging these competing pressures, providing clarity for leadership while amplifying the voices of those on the front lines of care.
Yet feedback means little if it begins and ends with a survey score. Its real strength lies in shaping a culture of listening and follow-through, where insights flow beyond dashboards and reach nurses, technicians, and front-desk staff who define a patient’s experience moment by moment. Closing the loop goes beyond an operational exercise; and becomes an act of empowerment that transforms scattered comments into practical changes and, ultimately, trust.
Harnessed well, patient feedback becomes both a safeguard for compliance and a catalyst for better care, proof that even in the most complex healthcare systems, small signals from patients can set a larger transformation in motion.
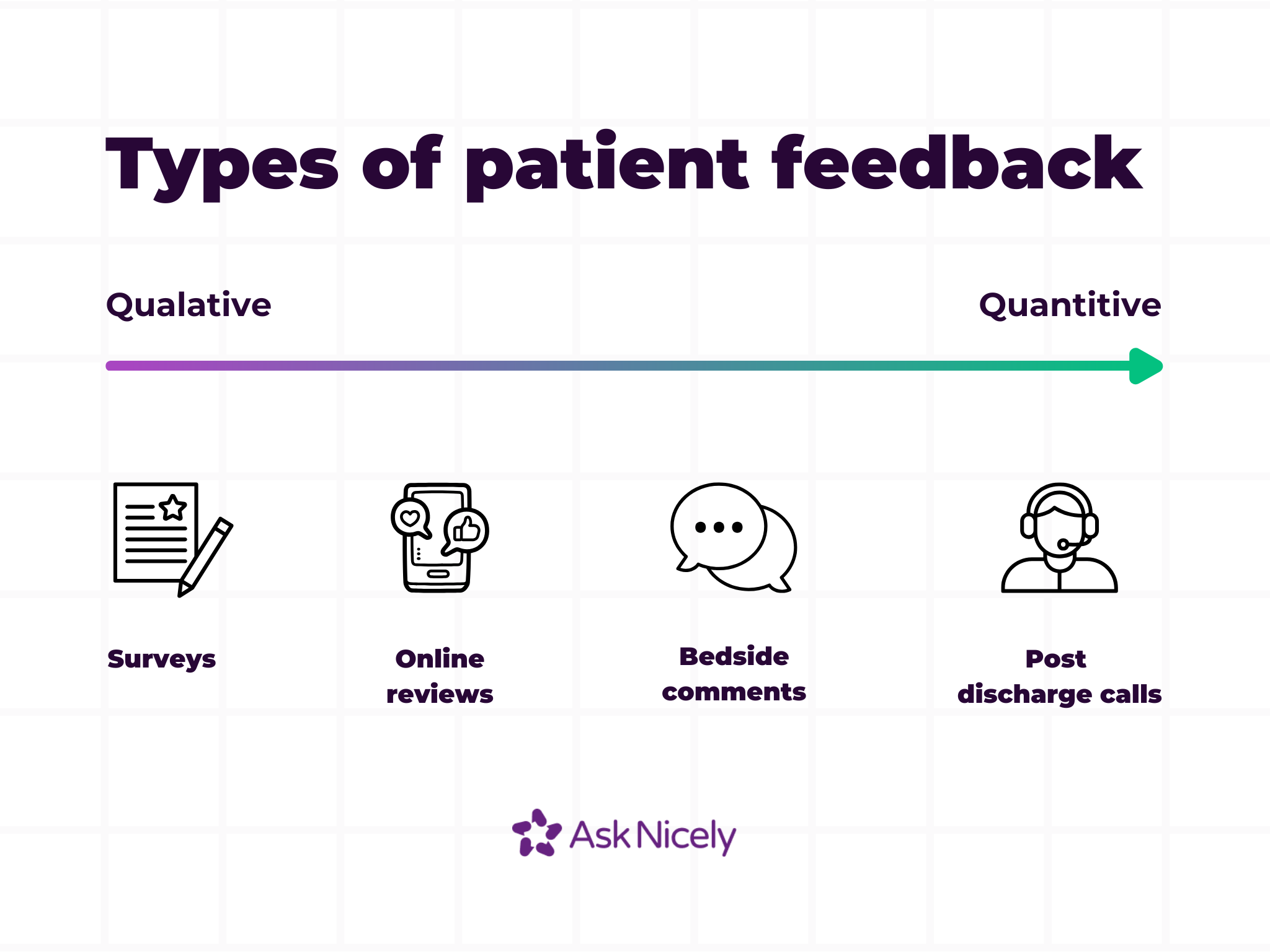
Patient feedback is what patients share about their care—honest impressions, feelings, and suggestions in their own words. It spans the clinical and the personal; survey scores, online reviews, bedside comments, follow-up calls, even a handwritten thank-you note. Modern healthcare increasingly treats this input as a core data stream, on par with infection rates, readmission figures, or other clinical quality metrics.
Where satisfaction often lags—showing how patients felt after the fact—feedback arrives closer to real time, offering clues that can prevent small frustrations from calcifying into systemic failures. Satisfaction is a snapshot; feedback is a moving picture. One signals whether expectations were met, the other provides the raw material to improve what comes next.
Different roles in a health system read patient feedback through different lenses. Operations leaders analyze it to pinpoint delays and inefficiencies. Marketing teams track it as a measure of reputation and public trust. Clinicians see it as a direct reflection of their care, communication, and bedside experience.
Healthcare has shifted from provider-led to patient-centered. People arrive informed, compare options online, and expect patient care that is not only clinically competent but also responsive and respectful. Feedback is no longer background noise; it is one of the few signals that speaks simultaneously to trust, loyalty, healthcare quality outcomes, and brand reputation.
Below are three core benefits that come up repeatedly when health systems embed patient feedback into daily practice.
Feedback uncovers care gaps and workflow friction before they escalate into adverse events or lower star ratings. For instance, at Schweiger Dermatology, 50% of providers improved their individual NPS scores by 12 points in just one year. Each provider receives real-time patient sentiment directly on their phones, desktops, and iPads, highlighting what they’re doing well and offering actionable insights on how to enhance the patient experience that very day.
Patients feel safer and more valued when they know their concerns don’t disappear into a black box. When feedback is acknowledged promptly and followed by visible, meaningful action, it creates a “heard and helped” effect. This not only improves patient sentiment but also strengthens loyalty and retention over time.
For example, a patient who sees their issue addressed (whether it’s a scheduling conflict, communication gap, or care question) is more likely to return and recommend the practice. Over time, consistently responding to patient feedback fosters a culture of transparency and responsiveness, turning routine interactions into trust-building moments and differentiating your practice in a competitive healthcare landscape.
Frameworks such as HCAHPS in the United States, CQC in the United Kingdom, and similar quality schemes elsewhere now place structured patient feedback alongside clinical outcomes in scoring hospitals. Properly captured and anonymized, feedback supports audits, demonstrates continuous improvement, and helps meet HIPAA or GDPR obligations around privacy.
Organizations that maintain a live feedback loop avoid the scramble before inspections. Patterns of praise and concern are already documented, actioned, and measured, evidence regulators value during accreditation reviews.
Collecting feedback is not just about sending a link every quarter. It is about access, inclusion, and making sure every voice has a way in. Relying on a single method risks skewing results toward the most vocal or digitally fluent patients. A mix of channels produces a fuller, more representative picture of care and supports equity goals that many health systems now prioritize.
Below are common approaches that work well when combined into a deliberate, system-wide strategy.
Surveys remain the backbone of patient feedback programs because they scale. A short text or email within 24–48 hours of a visit captures fresh impressions, while kiosk patient satisfaction surveys at discharge provide immediate insight. Keep them concise (one to three focused questions) and allow room for a brief comment. For example, a survey that includes a patient satisfaction score rating, as well as a follow up question on the best and worst part of their experience.
Patient portals already house lab results, visit summaries, and billing. Embedding a simple feedback form adds convenience for patients who prefer asynchronous communication. Integration with electronic health records allows comments to be captured directly alongside visit data, reducing manual entry and helping staff view feedback in the clinical context.
When survey data reveals a recurring pain point, small group discussions or one-on-one interviews help unpack the “why.” Recruiting participants across age, language, and socioeconomic lines ensures that solutions reflect the full patient population, not just the most engaged. These conversations often uncover system issues invisible in quantitative data.
Moments of care carry a freshness that fades quickly. Bedside tablets, waiting-room kiosks, or a QR code on discharge papers invite immediate impressions while details are still vivid. Real-time dashboards in AskNicely flag negative comments instantly, allowing staff to follow up before frustration hardens. Acting within hours, not weeks, can turn an at-risk experience into an expression of gratitude.
For all its value, patient feedback is not always easy to manage. Health and wellness care facilities wrestle with ownership questions, should it sit with the COO who oversees operations, the CX leader who tracks experience, or a shared service that centralizes reporting? The answer often shapes how problems surface and how quickly solutions reach the frontline.
Several common hurdles tend to appear across healthcare feedback systems. Each has practical fixes, many supported by tools like AskNicely that make feedback both easier to gather and easier to act on.
One of the biggest frustrations is hearing from too few patients. Timing is often the culprit: emails sent days after discharge are easy to ignore, while overly long surveys feel like homework. Mobile-first surveys delivered within 24–48 hours of a visit consistently perform better. Reminders add another lift without adding pressure.
Patients tune out when they are asked the same questions too often, or when surveys always reach the same demographic slice. Rotating question sets, spacing requests, and mixing methods (digital, in-person, portal-based) reduces fatigue and broadens representation.
Raw feedback can quickly become noise without clear filters or accountability. Frontline teams are easily overwhelmed when handed spreadsheets of comments that feel disconnected from daily work.
The fix is to distill insights into role-specific snapshots: executives see trend lines, operations managers see workflow gaps, and clinicians see patient comments relevant to their unit. AskNicely’s dashboards and automated workflows assign ownership, flagging which team should act and when.
Too many organizations treat HCAHPS or CQC feedback as a regulatory checkbox. The result is data collected for auditors rather than patients. When structured feedback is captured securely and acted on transparently, it builds trust with patients while satisfying HIPAA and GDPR requirements.
Collecting patient comments is only the first step. The real value emerges when an organization translates words and scores into decisions, workflows, and recognition that change the experience for the next patient.
As Julie Gessin, Chief Operating Officer at Schweiger Dermatology Group says “your feedback is only as good as your ability to act on it”.
Below are proven practices that turn raw input into measurable gains.
Acknowledging feedback signals respect. A quick note or call shows the patient that their experience was not filed away but acted upon. AskNicely automates close-the-loop workflows, routing each comment to the right person and prompting a response.
Nurses, technicians, and reception teams shape most patient interactions, yet they often see only lagging reports. Delivering bite-sized, role-specific insights helps them adjust in real time.
Positive feedback is an underused motivator. Publicly sharing praise boosts morale and reinforces behaviors worth repeating. To further drive customer-centric behavior, Caci (a leading provider of medical aesthetics services in New Zealand) has implemented an innovative incentive scheme called the "Caciverse." This program rewards customer-facing teams, such as estheticians and clinicians, for delivering exceptional customer experiences, as measured by positive feedback and NPS scores.
Feedback should map to the same metrics leadership tracks—quality, patient safety, satisfaction, and loyalty. Linking comments to KPIs keeps quality improvement work funded and visible. AskNicely connects qualitative and quantitative data, so leadership can see how addressing one complaint trend correlates with HCAHPS or CMS Star Ratings.
Treat feedback as an ongoing loop: collect data, analyze, act, and measure again. Small, regular adjustments outperform sporadic overhauls. AskNicely automates each stage, surfacing fresh insights weekly and tracking outcomes over time.
Large volumes of free-text comments can overwhelm human reviewers. AI can cluster themes, detect sentiment, and suggest priorities for improvement. With NiceAI, healthcare organizations can sift through all patient feedback in a matter of seconds, surfacing key trends and turning them into actionable insights.
Managing patient feedback at scale takes more than ad-hoc feedback surveys or spreadsheets. AskNicely turns every comment, score, and story into an actionable signal. Built for healthcare, the platform meets privacy obligations while empowering teams to act on what patients actually say.
Key capabilities include:
AskNicely makes patient feedback practical instead of burdensome: actionable for frontline teams, strategic for executives, and transparent for patients.
Ready to see what better listening looks like?
Book a demo and explore how AskNicely can help your teams turn every patient comment into progress.
Start with your goals, whether that means improving patient experience, lifting satisfaction scores, or meeting compliance requirements for healthcare services. Evaluate platforms on ease of use, integration with existing systems, and their ability to deliver actionable insights rather than raw data dumps. Look for features that support gathering patient feedback from new patients as well as in-patient populations, and check if the platform supports benchmarking so you can compare performance across clinics or departments.
Look for multi-channel data collection (SMS, email, kiosk) and multi-language support to reach all patient populations. High-quality real-time analytics and automated workflows help ensure every patient comment triggers appropriate action plans.
Recognition tools and dashboards linking feedback to KPIs help turn data into a culture shift. Clinics using role-specific dashboards often see higher staff engagement because feedback feels personal and actionable. Questionnaires should be flexible enough to capture insights from primary care and specialized services alike.
Modern platforms connect directly with EHRs such as Epic or Cerner to trigger feedback requests automatically after in-patient or outpatient encounters and with CRMs to track trends across the full patient journey.
For example, a primary care clinic might send a questionnaire through the patient portal immediately after a visit, with responses flowing into both the EHR and a central dashboard. This reduces manual work and ties every comment to a specific encounter, enabling better tracking of initiatives and action plans.
AI helps teams process large volumes of open-text comments from questionnaires, clustering themes, detecting sentiment, and surfacing trends quickly. Instead of reading thousands of responses, staff can focus on patterns like “wait times” or “staff communication” and act sooner.
Health systems can use AI to inform action plans and initiatives, such as adjusting staffing on weekends or improving patient experience across healthcare services. Case studies show that clinics using AI-driven insights often see measurable improvements in patient satisfaction scores.
Yes, if the platform is built for healthcare. Feedback data must meet the same standards as health information and medical records, with encryption in transit and at rest, role-based access, and audit logs. Systems should anonymize identifiers before analysis while preserving enough context for meaningful action plans, ensuring that both new patients and in-patient populations are protected.
A survey tool collects answers via questionnaires; a CXM platform turns those answers into action. CXM connects patient feedback to workflows, empowers staff with real-time insights, and tracks whether interventions improve key metrics. For instance, a basic survey might reveal patients dislike long wait times; a CXM platform routes that insight to the clinic manager, suggests operational initiatives, and tracks whether scores improve afterward. Clinics using benchmarking and action plans can see tangible results in improving patient experience across healthcare services.