Healthcare has always been about quality of care, but today, care also includes the quality of the experience. Patients have more choices than ever from hospital systems to specialist clinics to telehealth providers, and their expectations are rising. For healthcare leaders, this means patient experience is a critical differentiator tied directly to loyalty, referrals, and growth.
“Patient experience matters because patients have choices, especially today. And patients are really educated consumers, so the initial patient experience is going to define if they feel that this is a place that they want to or can go back to, or if they want to try to find something else,” said Julie Gessin, Chief Operating Officer at Schweiger Dermatology Group.
That’s where net promoter score (NPS) comes in. NPS offers a simple yet powerful way to measure patient trust and loyalty in real time. But here’s the catch: NPS isn’t valuable as just a number on a dashboard. Its true impact comes when patient feedback is shared with frontline teams, acted on quickly, and embedded into the culture of care.
So, let’s take a deeper dive into what NPS truly means for healthcare, how to measure it effectively, what benchmarks to aim for, and most importantly, how to turn it into daily actions that improve patient satisfaction and loyalty.
Net promoter score is a simple metric used across industries to gauge customer loyalty, but in healthcare, it carries a deeper significance. Here, it doesn’t just measure satisfaction with a service; it reflects the trust patients place in their providers and the likelihood they’ll recommend your practice, clinic, or hospital to friends and family.
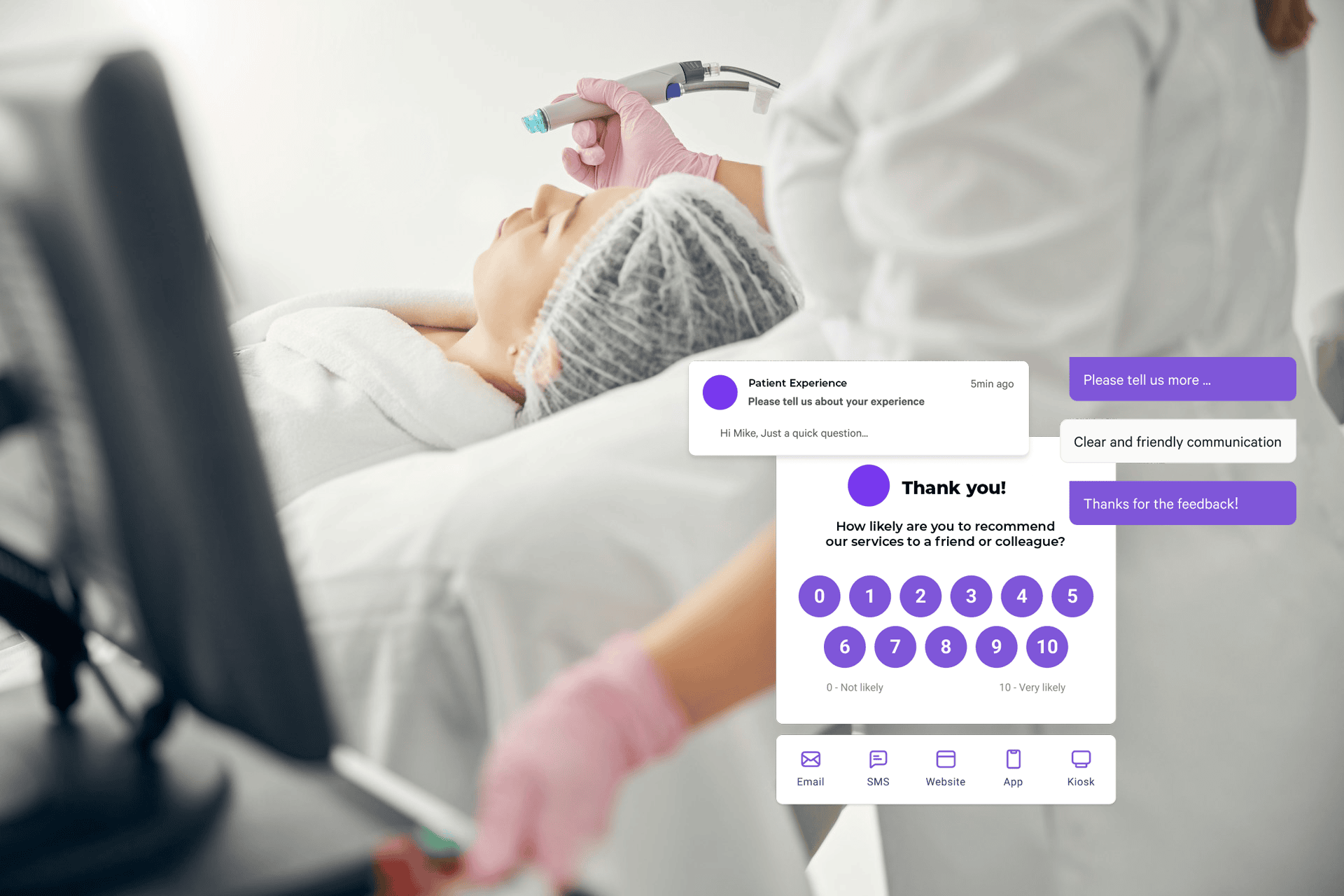
Unlike traditional, compliance-heavy surveys such as HCAHPS, which can take weeks or months to collect and analyze, NPS provides a fast, real-time snapshot of patient sentiment. Patients are asked a single, straightforward NPS question, typically, “How likely are you to recommend our care to a friend or family member?” and respond on a scale of 0 to 10. This simplicity makes it easier for patients to give feedback and for healthcare teams to respond promptly.
In healthcare, NPS can be applied at multiple touchpoints: immediately after a clinic visit, following a procedure, or even as part of ongoing care for chronic conditions. This flexibility allows organizations to track loyalty across the patient journey and pinpoint areas for improvement where it matters most.
By capturing feedback in real time and across diverse interactions, NPS offers healthcare providers a clear, actionable measure of patient loyalty and a tool to build stronger, trust-based relationships with the people they serve.
Measuring NPS effectively in healthcare is more complex than simply sending out a survey. The real power of NPS is in designing feedback processes that capture patient sentiment at the right moments, making it easy for patients to respond, and embedding insights into daily operations so frontline teams can act on them.
Here’s how to do it:
Not every interaction requires a survey. Identify key moments in the patient journey where feedback is most valuable, such as after a clinic visit, following a procedure, or at the conclusion of a treatment plan. These touchpoints ensure you’re measuring experiences that truly reflect patient loyalty and trust.
Healthcare patients are often faced with long compliance surveys, which can feel burdensome and reduce response rates. Short, timely NPS surveys (sent via email, SMS, or in-app) encourage participation and provide real-time insights. Platforms like AskNicely automate this process, delivering surveys at the right moment without adding administrative burden.
NPS measurement: NPS is calculated by categorizing patient respondents:
Subtracting the percentage of detractors from promoters gives your average NPS. This simple calculation provides a clear snapshot of patient loyalty.
Patient experiences can vary widely by department, visit type, or care team. Segmenting NPS results by these factors uncovers patterns and highlights where improvements are needed most. AskNicely’s analytics make this segmentation straightforward, helping healthcare leaders make data-driven decisions.
An NPS score is only valuable if it drives action. Share results with frontline staff in real time to enable the quick recovery of detractor experiences and recognition of promoters. Embedding NPS into daily operations ensures every team member understands their impact on patient loyalty and can continuously improve care.
Benchmarks give healthcare leaders a reference point to understand where they stand in comparison to peers and to set realistic improvement goals. Unlike industries such as retail or tech, where customer experiences are often more straightforward, healthcare involves complex, high-stakes interactions. As a result, NPS scores in healthcare tend to be lower on average, but that doesn’t mean they aren’t actionable or meaningful.
Commonly cited benchmarks for healthcare NPS include:
Average performers: Typically around 20 to 30.
Best-in-class providers: Often 50 or higher, depending on the specialty and healthcare setting.
It’s important to note that benchmarks in the healthcare industry vary by type of care. Elective procedures or outpatient clinics often see higher NPS scores because patients have more choice and control over their experience. Emergency care or complex hospital treatments may yield lower scores, reflecting the inherent stress and urgency of those situations rather than poor service.
Healthcare NPS scores usually lag behind other service industries, but that context doesn’t diminish their value. Benchmarks are useful as starting points, helping teams set targets and track progress. What matters most is the trend over time: are scores improving after interventions? Are patients increasingly likely to recommend your care? When approached this way, NPS becomes a tool not for comparison alone, but for continuous improvement and stronger patient loyalty.
NPS is a powerful tool that connects the overall patient experience to trust, reputation, and even financial performance. For healthcare organizations, it offers valuable insights that can drive real, tangible improvements in care delivery.
What makes NPS especially valuable in healthcare is that it can flow directly to frontline staff, not just executive dashboards. When doctors, nurses, and support teams receive timely feedback, they can celebrate promoters, address detractors, and continuously improve the patient experience. Embedding NPS into daily operations creates a culture of accountability and patient-centric care.
Patients who feel heard and valued are more likely to return and recommend your care to others. By tracking and acting on NPS feedback, healthcare organizations can strengthen trust and foster loyalty that lasts a lifetime.
NPS highlights areas where care can be improved, from communication and wait times to discharge processes. Acting on these insights leads to better patient experiences and, ultimately, better health outcomes.
NPS provides a clear, straightforward measure that unites all teams around one shared goal: improving patient loyalty and satisfaction. By focusing on a single metric that matters to patients, staff can prioritize what truly impacts the patient experience rather than getting lost in multiple, disconnected KPIs.
Positive patient experiences don’t just improve satisfaction, they drive tangible growth. AskNicely calls this “earned growth.” When patients have exceptional care experiences, they naturally refer friends and family, leave positive reviews, and continue returning for care, helping your organization grow without additional marketing spend.
NPS is a direct indicator of earned growth. High scores signal that patients are likely to recommend your healthcare services, boosting referral volume and enhancing your online reputation. Conversely, low scores highlight experiences that could harm patient retention or reduce word-of-mouth referrals. By tracking NPS over time and acting on feedback, healthcare organizations can turn everyday patient interactions into a consistent engine of growth.
Measuring NPS is just the first step; the real impact comes from taking action on what patients tell you. Improvement is where healthcare organizations turn feedback into better experiences, stronger loyalty, and tangible growth.
Here are practical, people-driven strategies for boosting NPS:
Patients want to feel heard. Following up with both promoters and detractors ensures their feedback leads to action. Quick, personalized responses show that your organization values patient input, which builds trust and encourages continued engagement.
Doctors, nurses, and administrative staff are the face of patient care. Providing them with immediate insights and coaching enables teams to improve interactions on the spot. Platforms like AskNicely deliver actionable feedback directly to staff, helping them refine communication and care delivery continuously.
Detractors represent patients at risk of churn or negative reviews. Addressing their concerns promptly through structured action plans can turn a poor experience into a positive one, reducing reputational risk and boosting loyalty.
Promoters are your advocates. Celebrating their positive feedback not only reinforces good practices but also motivates staff and strengthens the culture of patient-centric care.
While NPS captures loyalty, other metrics provide complementary insights. CSAT highlights immediate satisfaction, and HCAHPS ensures compliance and regulatory alignment. Using NPS data alongside these metrics gives a more complete picture and guides smarter improvements across the patient journey.
Collecting feedback is only valuable if it drives meaningful change—a challenge Healthie, a practice management platform for health and wellness providers, faced firsthand. “We weren’t struggling to collect feedback, but we needed a better way to connect it to overall business insights,” says James Kase, associate director of revenue operations at Healthie.
Before AskNicely, multiple teams had access to feedback, but it was difficult to centralize, analyze, and act on it. Since implementing AskNicely, Healthie has streamlined feedback collection, gained real-time insights, and empowered teams to address issues quickly. The platform also supports data-driven decision-making, helping prioritize product updates based on actual user needs.
The results speak for themselves: Healthie has improved customer satisfaction, retention, and engagement while reducing the time spent on manual feedback management by two to three hours per week. By transforming feedback into a strategic asset, Healthie ensures every user feels heard, fostering a company-wide culture of continuous improvement.
Read the full Healthie success, and more AskNicely case studies here.
Healthcare organizations that excel in patient experience have one thing in common: they act on feedback, and fast. AskNicely is designed to turn NPS into daily, frontline action, helping staff deliver better care while improving patient loyalty and organizational performance. Key features include:
By embedding feedback into daily routines, AskNicely helps healthcare providers not only measure loyalty but actively improve it, creating better patient experiences, stronger teams, and meaningful, earned growth.
Book a demo to see how AskNicely can help your organization turn patient feedback into real-time action.
In healthcare, a good NPS typically ranges from 20 to 30 for average performers to 50+ for best-in-class providers, depending on the specialty and care setting. Elective clinics or outpatient centers often see higher scores, while emergency or high-acuity care may score lower due to the complexity of patient experiences. The key is tracking improvement trends over time rather than focusing solely on the number.
Healthcare involves high-stakes interactions, complex procedures, and emotionally charged situations. Unlike retail or hospitality, patients may judge their experience based on outcomes, wait times, or stress levels beyond the provider’s control. This makes incremental improvements slower and requires a focus on both operational efficiency and patient-centered communication.
Frequency depends on touchpoints. Many providers survey after each visit or procedure, ensuring feedback is timely and actionable. For ongoing care, quarterly or semi-annual patient surveys may be appropriate. The goal is to balance capturing real-time insights with avoiding survey fatigue.
Yes. HIPAA compliance is achieved by anonymizing responses or storing identifiable information securely, with limited access to patient data. Platforms like AskNicely are designed to meet privacy standards while still delivering actionable feedback to care teams.
Common errors include: sending satisfaction surveys or questionnaires at the wrong touchpoints, treating NPS as a dashboard metric only, ignoring detractors, and failing to close the feedback loop with patients. Another frequent mistake is not segmenting scores by department or visit type, which hides actionable insights.
High NPS scores indicate loyal patients who are more likely to refer friends and family or leave positive online reviews. Studies show that a 1-point increase in NPS can translate to measurable growth in referral volume and retention, making it a practical tool for earned growth.
Share results in digestible, actionable formats, such as daily alerts for feedback relevant to each staff member or team. Highlight key takeaways like detractor experiences to resolve or promoter comments to celebrate rather than presenting raw dashboards. Automated platforms like AskNicely make this process seamless.
All three levels provide value. Provider-level NPS helps improve individual performance, department-level scores highlight systemic issues, and organization-wide NPS tracks overall patient loyalty trends. Segmenting scores ensures insights are actionable at the right level.
Sudden drops in NPS often reflect operational bottlenecks, like long wait times, staff shortages, or scheduling issues. Tracking NPS trends alongside operational data allows leadership to pinpoint and address the root causes of patient dissatisfaction.