
Every hospital has a patient journey map, but few have one that can change day-to-day experiences for patients. Long wait times, confusing communication, and missed follow-ups erode trust and leave leaders wondering why satisfaction scores and outcomes aren’t improving.
The healthcare industry has fallen behind others when it comes to designing experiences that feel clear, personalized, and convenient. Patients book flights, shop online, or even order coffee with seamless digital tools, then face a fragmented maze when navigating their care. Expectations have shifted, but the way most organizations approach patient journey mapping hasn’t kept pace.
That’s why mapping the patient experience effectively is so important. Done right, journey mapping forces teams to see every stage of care through the patient’s eyes, uncover hidden friction points, and align improvements with both clinical outcomes and regulatory requirements. Patient journey mapping is a framework for building trust, boosting retention, and meeting the rising bar set by CMS star ratings, HCAHPS surveys, and other benchmarks.
With that said, let’s explore the practical side of patient journey mapping: the key steps to build a map that actually works, examples from healthcare organizations that are getting it right, and best practices to ensure your efforts don’t stop at the whiteboard.
You’ll also see how continuous feedback and frontline action, powered by tools like AskNicely, can turn static maps into living systems that drive measurable improvements.
At its core, patient journey mapping is a structured way to visualize every step a patient takes when engaging with a healthcare organization, from the moment they search for a provider to their post-treatment follow-up. Unlike an internal process diagram, which focuses on what staff do behind the scenes, a journey map centers on the patient’s lived experience: their actions, emotions, expectations, and frustrations. The goal is clarity, making the invisible visible so teams can see care as patients actually experience it.
Originally, journey mapping was used in industries like retail and technology to design better customer experiences. In healthcare, however, the practice has evolved into something far more significant: a dynamic operating model. A patient journey map is no longer just a design tool; it becomes a framework for coordinating care, aligning teams, and measuring the impact of improvements across touchpoints.
Consider a typical patient journey for someone scheduling elective surgery. It begins with online research and appointment booking, moves through pre-admission instructions and check-in, includes the surgery itself and the recovery process, and extends into follow-up visits, billing, and ongoing communication.
A complete journey map outlines these stages and captures critical details, like the anxiety a patient feels while waiting for test results or the relief of clear discharge instructions. By layering these emotional moments alongside operational steps, the map highlights the “moments that matter” most in building trust.
This patient-centered perspective is what differentiates journey mapping from standard process flows. It pushes organizations to ask: What does the patient value here? Where do we create confidence, and where do we introduce confusion or risk? Answering these questions uncovers opportunities to improve both experience and outcomes.
Importantly, patient journey mapping is distinct from customer journey mapping in other industries. Healthcare journeys are shaped not just by convenience and service quality, but by complex emotions, strict regulatory requirements, and the involvement of multiple stakeholders, including patients, caregivers, clinicians, and insurers. The stakes are higher, and the impact of getting it right extends well beyond satisfaction into measurable health outcomes.
Patient care is among the most high-touch, emotionally charged industries to exist. Patients are more than consumers, they’re individuals navigating moments of vulnerability, uncertainty, and hope.
A well-constructed journey map highlights the friction points patients encounter every day, whether it’s waiting weeks for an appointment, struggling with unclear billing, or receiving inconsistent follow-up instructions. When these issues are surfaced and addressed, organizations see direct gains in patient satisfaction scores and loyalty metrics. Improvements at these “moments that matter” reduce churn, drive positive word-of-mouth, and fuel earned growth.
Journey mapping is also about operational precision. By charting touchpoints, organizations can reduce no-shows with clearer pre-visit instructions, smooth discharges to minimize readmissions, and standardize handoffs between departments. When journeys are smoother, patients are more likely to follow treatment plans, and staff experience fewer errors and less duplication of work, helping reduce burnout. These efficiencies ultimately reinforce both retention and referrals.
Patient journeys don’t follow departmental boundaries. Instead, they cut across scheduling, clinical care, billing, and follow-up. Without a shared framework, teams often optimize their own processes while unintentionally creating friction elsewhere.
A journey map makes those misalignments visible, giving staff a common language to design improvements collaboratively. When paired with real-time feedback platforms like AskNicely, frontline teams can immediately see where a patient’s experience is breaking down and take action in the moment. As a result, this improves outcomes for patients and strengthens their loyalty by reducing confusion and delays.
For journey mapping to stick, it must resonate with leadership. Executives want to see evidence that investments in patient experience lead directly back to retention, lifetime value, and cost-to-serve. A robust journey map provides that line of sight: fewer missed appointments, lower costs, streamlined communication reduces rework, and better experiences drive repeat visits and referrals. Framing journey mapping as both a patient-centered and financially sound strategy ensures it earns the resources and attention it deserves.
Breaking the patient journey into stages is essential for one simple reason: experiences are rarely won or lost all at once. Instead, they hinge on a series of touchpoints, each with its own opportunities and risks. By mapping these stages clearly, organizations ensure they don’t overlook the “small” moments that add up to trust, loyalty, and better outcomes.
It’s also important to recognize that journeys are not uniform. A patient managing a chronic condition has very different needs and expectations than someone seeking emergency care or a cosmetic procedure. Benchmarks, friction points, and even emotional intensity vary by patient. The framework below provides a common structure, but teams should adapt it to reflect their patient mix.
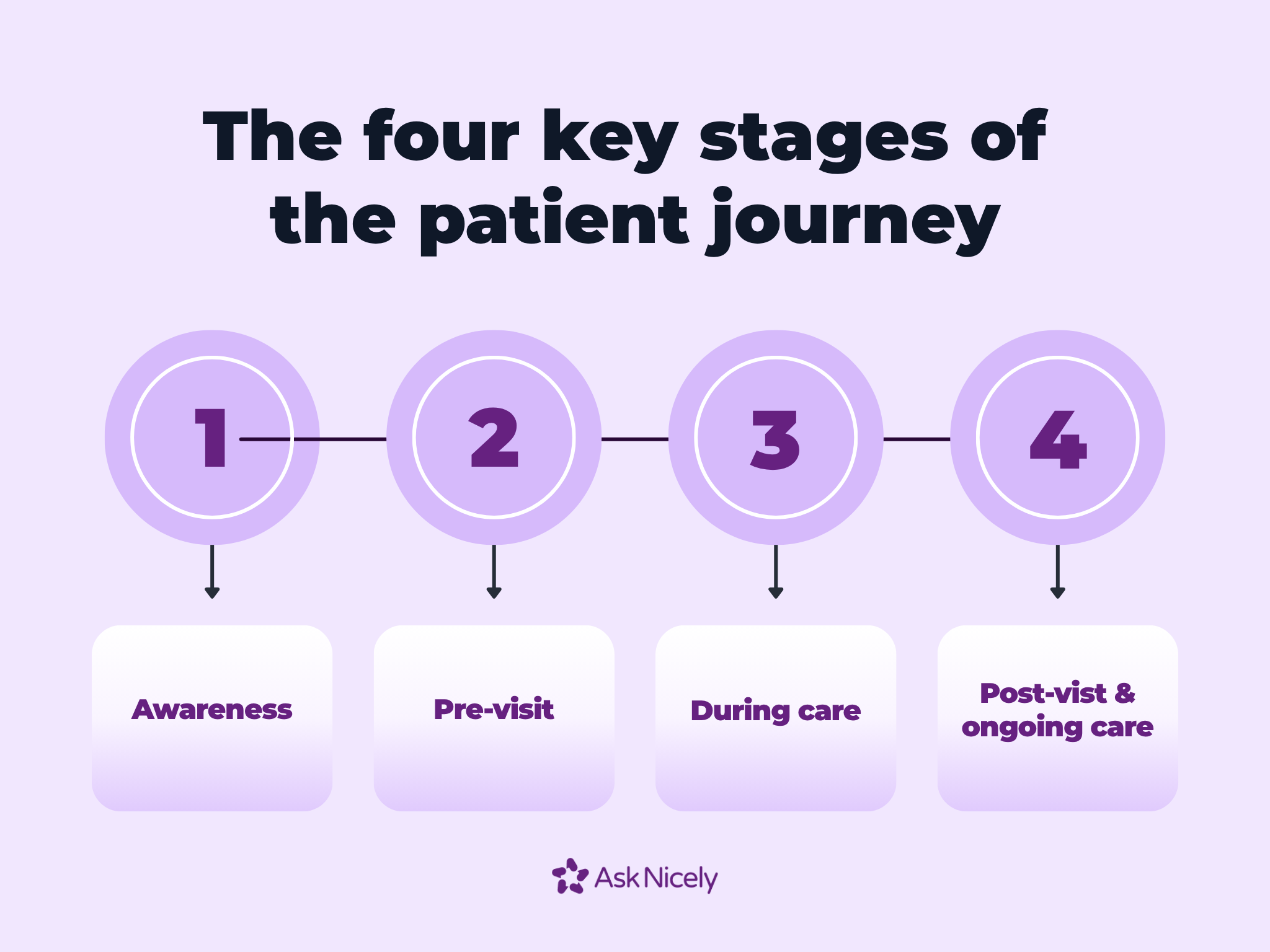
The journey begins before a patient ever sets foot in a clinic or hospital. Finding a provider, checking insurance coverage, and researching options online all shape early impressions. If access feels complicated by limited availability, poor digital tools, or unclear insurance information, patients might disengage before care even begins. A streamlined awareness and access stage builds confidence and reduces churn from the outset.
Once a patient has chosen a provider, scheduling and pre-visit communication become critical. Do patients receive timely confirmations and reminders? Are forms easy to complete digitally, or do they face stacks of paperwork at check-in? Clarity at this stage reduces no-shows, eases anxiety, and sets the tone for the visit.
The clinical encounter is the centerpiece of the journey, but it’s not just about medical expertise. Empathy, clarity in communication, and the overall environment all play decisive roles in how patients perceive care. Staff engagement matters too, patients can sense when clinicians are overworked or disconnected. A supportive environment reinforces trust and directly influences adherence to treatment plans.
The journey doesn’t end when a patient leaves the exam room. Billing transparency, follow-up calls, test result communication, and care management for chronic conditions all shape the ongoing relationship. Mishandled post-visit steps are a leading cause of dissatisfaction, while clear and compassionate follow-up builds loyalty and turns patients into advocates who share positive experiences with others.
Patient journey mapping is not a one-size-fits-all exercise. It requires a structured process that blends data, empathy, and continuous iteration. When done thoughtfully, a journey map is the blueprint for improving patient experience, operational efficiency, and clinical outcomes.
Here’s a step-by-step approach to building a map that drives measurable results.
The foundation of any journey map is real patient data. Assumptions and anecdotal feedback can only take you so far. Quantitative insights, like survey responses, NPS scores, or CSAT ratings, reveal trends and highlight problem areas at scale. Meanwhile, qualitative insights, like interviews, focus groups, or patient shadowing, capture emotions, context, and unmet needs. AskNicely makes gathering real-time, scalable feedback straightforward, ensuring your journey map reflects the voices of actual patients rather than internal perceptions.
Not all patients experience care the same way. New patients, returning patients, chronic-care patients, and acute-care patients all have distinct needs. Creating patient personas allows your team to design tailored journeys that avoid generic assumptions. Mapping touchpoints for each persona, from appointment scheduling to follow-up communication, helps highlight where improvements will have the greatest impact.
Functional steps alone do not define the patient experience. Emotional highs and lows, like anxiety before surgery, relief after receiving a clear diagnosis, or confusion during billing, can dramatically influence loyalty and satisfaction. Identifying these “moments that matter” ensures teams prioritize interventions that resonate with patients on both an emotional and operational level.
A clear visual representation makes the journey map actionable for both staff and executives. Formats can include linear timelines, swimlanes, or service blueprints. While static diagrams often end up tucked away in presentations, AskNicely dashboards and leaderboards bring the map to life. Frontline staff gain real-time visibility into patient feedback, enabling continuous improvement and accountability at every stage of the journey. By connecting abstract maps to tangible actions and daily insights, organizations turn mapping from a project into an operational system.
Customer journey worksheet: Dental and medical: Use this worksheet to map out the points of contact with a patient at a dental or medical practice.
Healthcare journey maps face the task of balancing empathy with compliance. HIPAA privacy safeguards, CMS star ratings, quality standards, and billing transparency are all integral to patient experience. Overlooking compliance can introduce unwanted friction to the experience. Patients frustrated by unclear consent forms or privacy lapses will disengage quickly. Organizations that integrate regulatory requirements into journey mapping not only reduce risk exposure but also reinforce patient trust.
A journey map is never truly finished. Co-creation with frontline staff and patient representatives ensures accuracy and relevance. Cross-functional review sessions and ongoing iterations keep the map current as processes, patient expectations, and regulations evolve. The result is a living tool that guides teams, informs leadership decision-making, and sustains meaningful improvements across the organization.
Patient journey maps have the potential to transform healthcare delivery, but they are not immune to pitfalls. Many organizations invest in mapping exercises that look impressive in boardrooms but fail to influence day-to-day operations. Without clear ownership, robust data and analytics, and ongoing follow-through, even the most detailed maps can stall. Below are some of the challenges teams frequently encounter.
Patient journeys often span multiple departments, including scheduling, clinical care, billing, and post-visit follow-up. Without a designated owner or cross-functional collaboration, maps can become disconnected from the realities of daily operations. When no team is accountable for acting on the insights, friction points persist, and improvements stall.
A map is only as good as the data behind it. Many healthcare organizations rely on fragmented feedback, collected in different systems, at inconsistent times, or focused on narrow stages of care. The result is a partial view that misses critical pain points, leaving teams to make decisions based on assumptions rather than real patient experience.
It’s easy to create a visually detailed journey map that impresses stakeholders but overwhelms staff. Overly complex maps or static diagrams often get tucked away in presentations and never become actionable. If a map doesn’t clearly highlight key touchpoints and moments that matter, it fails to guide improvements.
Even when teams have a clear map and robust feedback, turning insights into action is another challenge. Staff may understand pain points but lack the tools, authority, or real-time visibility to address them. Without mechanisms to close the loop, journey maps remain conceptual rather than operational.
Finally, some organizations treat the creation of a journey map as the endpoint rather than the starting point. Mapping is a diagnostic tool, not a substitute for process redesign, staff training, or continuous improvement. Failing to treat the map as part of an ongoing management system can result in minimal impact on patient experience and organizational outcomes.
While patient journey mapping can be transformative, its success depends on how it’s executed. The following best practices provide practical guidance for turning maps into actionable, measurable improvements and highlights how AskNicely helps healthcare organizations operationalize patient-centered insights.
The most effective maps focus on patient needs, emotions, and expectations, not just internal workflows. Empathy-mapping exercises, interviews, and patient shadowing help teams identify emotional highs and lows that drive loyalty and satisfaction. By prioritizing the patient perspective, organizations uncover the “moments that matter” and design interventions that truly improve experience.
Journey mapping is a collaborative process. Engaging staff at every level ensures the map reflects reality, not assumptions. Frontline insights often reshape maps in ways executives alone cannot anticipate, from identifying friction during check-in to clarifying discharge instructions. Co-creation builds buy-in and ensures improvements are feasible and effective.
A journey map achieves impact only when tied to measurable outcomes. Satisfaction scores, NPS, loyalty, and retention metrics help teams identify which interventions work. AskNicely provides real-time dashboards that connect journey touchpoints to KPIs, making it easy to monitor progress and quantify ROI over time.
Patient expectations, technology, and regulatory requirements evolve continuously. Effective maps are revisited regularly, on a quarterly or annual basis, to reflect these changes. By updating maps in line with real-time feedback and frontline input, organizations ensure they remain relevant and actionable.
Journey mapping is not a one-off project; it’s an ongoing operational discipline. Feedback loops, staff coaching, and iterative changes embed improvements into daily practice. AskNicely helps healthcare teams close the loop by surfacing insights in real time, enabling staff to act, and tracking the effect of changes, so improvements stick across the patient journey.
Journey maps should guide coaching, recognition, and accountability at the staff level. By linking each stage of the patient journey to specific frontline behaviors, whether greeting patients with empathy, clarifying instructions, or following up after discharge, organizations create a culture where experience improvements are measurable, repeatable, and sustainable.
Creating a patient journey map is an essential step, but maps alone cannot transform the patient experience. Real impact comes from tools that turn insights into action. AskNicely bridges that gap, taking journey mapping from a static visualization to a living system that drives daily improvements across your organization.
Healthcare providers use AskNicely to capture feedback at every touchpoint, coach frontline staff, and measure results across the entire patient journey.
Standout features include:
Patient journey mapping is the starting point. AskNicely ensures it becomes an operational advantage.
Book a demo to see how AskNicely can turn your journey maps into measurable, real-world improvements.
The most effective tools combine real-time feedback, analytics, and operational workflows. Platforms like AskNicely allow healthcare teams to link patient insights directly to frontline actions, coach staff, and monitor KPIs like NPS, CSAT, and retention. Unlike static diagrams, these tools turn abstract maps into living systems that continuously improve experience and outcomes.
Journey maps should be reviewed regularly, typically quarterly for high-touch updates and annually for strategic overhauls. Updates should reflect changes in technology, patient expectations, regulatory requirements, or operational processes. Continuous refinement ensures that maps remain accurate, actionable, and relevant to staff and patients alike.
Key metrics include patient satisfaction scores, NPS, CSAT, loyalty, retention, appointment adherence, and readmission rates.
Patient feedback software captures insights at every touchpoint, from pre-visit communication to post-discharge follow-up. By consolidating quantitative and qualitative data, it reveals pain points and emotional highs and lows. Tools like AskNicely also provide dashboards, leaderboards, and coaching workflows, ensuring insights translate into actionable improvements.
Yes. When staff see how their actions directly impact patient satisfaction and outcomes, engagement rises. Co-creating maps with frontline teams also fosters ownership and cross-functional collaboration, reducing burnout by clarifying responsibilities and aligning workflows with patient-centered goals.
Traditional survey tools collect data but rarely connect it to operational action. Journey mapping software goes further by visualizing the patient experience, highlighting key touchpoints, and integrating real-time feedback into workflows. AskNicely, for example, enables coaching, accountability, and continuous improvement, bridging the gap between insights and measurable results.
NPS and CSAT quantify patient loyalty and satisfaction at critical moments. Integrating these metrics into journey maps allows teams to track improvements over time, measure the impact of interventions, and prioritize changes at touchpoints that most influence patient perception and retention.
AskNicely provides a scalable platform to capture feedback across multiple sites and touchpoints. Real-time dashboards, automated survey distribution, and coaching workflows allow organizations to act on insights immediately, ensuring that journey maps evolve from static diagrams into operational tools that improve patient satisfaction, loyalty, and outcomes.
Absolutely. AI and predictive analytics enhance journey mapping by identifying trends, forecasting risk points, and personalizing experiences. However, maps remain essential for visualizing care from the patient's perspective and guiding interventions. AI works best when layered on a strong, patient-centered journey framework.
The most frequent mistake is treating mapping as a one-time exercise. Organizations create detailed maps but fail to act on them, integrate them into workflows, or update them as processes evolve. Without follow-through, the map becomes a static artifact rather than a tool for continuous improvement and measurable patient impact.